Posters


Does ability to access health care vary with personal and social characteristics?
SAPC Conference, Exeter UK
July 04, 2019
Context and aim: Interventions to enhance access tend to benefit persons who are better-off rather than the disadvantaged, possibly due to socially-related differences in access abilities. The Patient-Centred Accessibility Framework suggests that variations in access to primary healthcare can be due to differences in how healthcare services are organized OR in the variations in the abilities of people to access care (ability to perceive need, to seek appropriate options, to reach services, to pay and to engage in a clinical encounter). Our participatory action-research program co-designed, piloted and evaluated interventions to increase access to comprehensive primary health care for socially vulnerable populations in six jurisdictions: three in Canada and three in Australia. We explored how access abilities correlate with indicators of poor access and how they vary with personal and social characteristics.
Approach: Although the vulnerable populations and interventions were different in each site, all interventions used a common evaluation method. Pre-and post-intervention surveys incorporated the same: indicators of poor access (reported difficulties accessing care, emergency room use); proxy measures of access abilities and personal and social characteristics (financial status; education; social support; language proficiency; immigrant/refugee status; chronic illness burden). This is a pooled analysis of the baseline data in the 284 participants across the six study regions. We explored correlations between access abilities and self-reported access problems; then access abilities with personal and social characteristics.
Results: Referring to the last 6 months, 38% of persons reported having difficulties with getting needed healthcare or advice, which in 2/3 resulted in forgone care; 29% of the participants reported using the emergency room, of which 42% attributed use to access difficulties. Lower scores for each of the access abilities are associated with statistically significant increase in the likelihood of reporting difficulties with access and use of the emergency room. There is no difference in access abilities by age, sex, chronic illness burden. Lower access abilities are associated (in decreasing order) with poor financial status, low social support, limited language proficiency, low education. When these social characteristics were summed into an index, higher social vulnerability correlates with lower ability to perceive (r=-0.25), to seek (r=-0.23), and to engage (r=-0.36, r=-0.23) and more experienced cost barriers (r=0.16) but not with ease of travelling to regular clinic (reach).
CONCLUSION: Lower patient abilities to successfully navigate all the stages of the care-seeking trajectory is associated with difficulties with accessing care and potential overuse of emergency rooms. These limited access abilities are more evident in socially vulnerable populations – a clear example of healthcare inequity. Primary healthcare access can become more equitable and appropriate by organizing services to be more attentive to persons with poor access abilities, which is likely to benefit especially the socially vulnerable.

Enhancing access to care through a pop-up model of service delivery: Service provider practice changes and organizational policy implications
CAHSPR Conference, Halifax
May 29, 2019
Background and objectives: The Alberta Local Innovation Partnership (LIP) of the Innovative Models Promoting Access-to-Care Transformation (IMPACT) research project designed and implemented pop-up health and community services events in Lethbridge, Alberta. The pop-up events brought together primary healthcare (PHC) service providers to provide care in different locations to people who are underserved by, and struggle to connect with, PHC services.
Approach: Participatory action research (PAR) approaches were used to design and implement the pop-up events. We worked closely with PHC service providers to improve the engagement and approachability of services at the pop-ups. Over the course of the research program, trying and learning informed improvements to the pop-up model that impacted service provider practice. These included shifting from designated ‘navigators’ to incorporating navigation in everyone’s role, practicing warm handoffs, coming out from behind your table, and using plain language signage and materials. Service providers attended planned rehearsals before each pop-up event where these improvements to the pop-up model were introduced.
Results: Follow-up interviews with service providers revealed that they had embraced the ideas introduced at the pop-ups to provide care differently. Service providers said they individually adopted new ways of practicing navigation, warm handoffs, and using new tools to improve engagement and approachability. Further, service providers reported advocating with their leadership for more far-reaching changes, such as expanding outreach , recognizing the unique needs of vulnerable populations (e.g., transportation), and improving referral processes.
Conclusion: The pop-up model for PHC service delivery has improved access to PHC by promoting changes in the way service providers provide care. New and creative ways of providing care were introduced and tested. Service providers adopted many of these ideas within their organizations, influencing operational and programmatic policy changes.

Need help navigating the health system? Mixed Methods Evaluation of a Lay Volunteer Telephone Service to Support Patient Navigation in Quebec
CAHSPR Conferene, Halifax
May 29, 2019
Background and objectives: To address the important number of patients without a family physician, the Quebec Ministry of Health created a centralized waiting list. Evidence shows that patients from disadvantaged neighbourhoods often stay longer on the waiting list (≥ 3 years) and face multiple barriers in connecting with a family physician. We present results from the evaluation of this innovative intervention implemented in two Quebec regions to facilitate the attachment of vulnerable patients through the centralized waiting list.
Approach: IMPACT is a 5-year Canada-Australia research program aiming to co-design, implement and evaluate interventions to improve access to primary healthcare (PHC) for vulnerable populations. In Quebec, a partnership of physicians, researchers and decision-makers developed a telephone support service offered by lay volunteers to help patients from disadvantaged neighborhoods on the centralized waiting list connect with their newly assigned family physician. The service helps patients prepare for their appointments and addresses access barriers. Evaluation: Mixed-methods approach using interviews (n=19) and surveys pre/post intervention (n=59). Outcomes measures and themes were conceptualized & integrated based on Levesque et al.’s access framework (2013).
Results: Outcomes are measures and themes conceptualizing access to PHC (Levesque, Harris, Russell 2013) including, in particular “approachability” and “appropriateness”. The service improved patients’ “ability to reach” and “ability to engage”: it helped patients access the right service at the right place at the right time. The personal approach of the navigation service, by a lay volunteer, creates the foundation for a positive and enduring patient-physician relationship, leading to decreased emergency department use for minor care, lower likelihood of unmet needs and increased likelihood of successful patient-physician attachment. Volunteers provide appreciated support to PHC clinics physicians and staff by alleviating feelings of work overload and contribute to fostering positive feelings in disadvantaged patients towards their newly assigned PHC clinics and physician.
Conclusions: Lay volunteers are a low cost resource that facilitate patient-physician attachment and enduring relationships between patients and family physicians. This intervention proves to be a particularly beneficial approach to improve access to PHC for patients from disadvantaged neighborhoods who may face barriers to accessing healthcare.
Driving Organizational Innovation in Primary Health Care Though Multi-Stakeholder Partnerships
Family Medicine Forum, Toronto
November 14, 2018
-
Emphasis on partnerships in primary health care has recently increased, with health care reforms globally integrating ideas about partnerships and collaboration.
-
Effective partnerships mobilize complimentary knowledge and expertise of partners, resulting in outcomes greater than those achieved working individually.
-
Despite extensive literature on processes and approaches that enhance partnership effectiveness, evidence demonstrating links between the implementation of these approaches and the achievement of desired outcomes is still insufficient.
-
This research addresses this gap in the context of care transformation in primary health care. It informs future policy and decision-making, to guide and assess the value of partnerships in improving the organizational aspects of primary health care.
Trusting and Trying: Innovating in the Community
NAPCRG Conference, Chicago
November 12, 2018
The Alberta, Canada LIP worked with multiple stakeholders to design and implement a Pop-up Health and Community Services Event for residents of north Lethbridge. A pop-up is an event that brings together primary health care service providers in a shared, conveniently located space. The intervention had several important impacts on primary health care providers and practices.
Person-Centred Care in an Australian Hospital Avoidance Program: A Qualitative Study of Participants’ Experiences
NAPCRG Conference, Chicago
November 12, 2018
Hospital avoidance programs aim to reduce hospital demand for people who present frequently to hospital. A core principle is person-centred care enabled by a collaborative and respectful relationship between the provider and person.
Monash Health's Complex Care Program supports people frequently presenting to hospital to get back to the community through a structured and proactive approach. In this poster, we examined to what extent person-centred care is incorporated into the Complex Care Program.
Driving Organizational Innovation in Primary Health Care Through Multi-Stakeholder Partnerships
NAPCRG conference, Chicago
November 12, 2018
-
Emphasis on partnerships in primary health care has recently increased, with health care reforms globally integrating ideas about partnerships and collaboration.
-
Effective partnerships mobilize complimentary knowledge and expertise of partners, resulting in outcomes greater than those achieved working individually.
-
Despite extensive literature on processes and approaches that enhance partnership effectiveness, evidence demonstrating links between the implementation of these approaches and the achievement of desired outcomes is still insufficient.
-
This research addresses this gap in the context of care transformation in primary health care.
Efficacy of an Innovative Primary Care Based Approach to Address Equitable Access to Resources in the Community: The ARC-Navigation Model
NAPCRG Conference, Chicago
November 12, 2018
Health enabling community resources, such as smoking cessation, falls prevention, self-management programs, and caregiving support, are underused. Social factors, such as transportation, language, literacy, and finances pose barriers to their access. Patient Navigator programs (where a person is tasked with helping connect patients to community resources) have been demonstrated to be useful in supporting patients access resources they need, and promote equity in specific medical contexts (e.g. cancer) and for specific communities (e.g. immigrants).
Very little is known about whether a Patient Navigator program integrated within primary care (PC) can help address the diverse access needs of the general population. In this study, we assessed the efficacy of the ARC-Navigation Model to enhance equitable Access to Community Resources.
“Need Help Navigating The Health System?” Quebec’s Experience in Using a Participatory Action Research Approach to Implement a Lay-Volunteer Telephone Support Service
NAPCRG Conference, Chicago
November 10, 2018
In Québec 20% of the population does not have a family physician and are on a centralized waiting list waiting to be assigned to a primary care physician. We found that patients in disadvantaged neighborhoods wait longer on the waiting list and are more likely to be returned to the list. Using a participatory action research (PAR) approach, we co-designed, implemented and evaluated an intervention with decision makers, healthcare system leaders and physicians to address this issue.
Our objective was to evaluate if a pilot intervention helped disadvantaged patients from the waiting list to connect with their newly-assigned family physician, to reduce unmet needs for care, and to increase their autonomy to navigate the healthcare system.
Increasing Access to Care Through Shared Space: Space is Not Enough
NAPCRG Conference, Chicago
November 10, 2018
The Alberta IMPACT research team used a four-part ecological model to guide the implementation of a pop-up health and community services event for people who are underserved by, and struggle to connect with primary healthcare services. Th objectives were to create an opportunity for attendees of the pop-ups to access multiple services in one easy to access, temporary location and improve collaborative care among service providers by encouraging collaborative practice and sharing of resources. This poster examines the significance of space on service providers and attendees of the pop-up.
Pop-Up Inspirations for Change: Service Providers Reflect on Knowledge, Attitudes, and Behaviours to Improve Access to Care
NAPCRG Conference, Chicago
November 10, 2018
Using a participatory action research approach, the Alberta Local Innovative Partnership located in Lethbridge, Alberta, Canada worked with community stakeholders to design and implement a pop-up intervention to enhance access to care for people who are underserved by, and struggle to connect with, primary health care services. This poster describes changes to providers' knowledge, attitudes and behaviour after participating in the pop-up.
Person-Centredness in a Complex Care Program: Perspectives of Clients and Staff
PHCRIS Conference, Melbourne
August 01, 2018
The Complex Care Program of Monash Health supports people frequently presenting to hospital to get back into the community through a structured and positive approach. Care coordinators, nurse practitioners, medical specialists and allied health staff work together to meet the needs of those with chronic heart failure, chronic respiratory disease and complex psychosocial needs.
Because little is known about the experience of people with chronic and complex needs in hospital avoidance programs, we aimed to examine the extent to which person-centred care is incorporated into the Complex Care Program.
Perspectives of Vulnerable People and Care Providers on Challenges to Access Primary Health Care: A preliminary qualitative analysis
CAHSPR conference, Montreal
May 29, 2018
This presentation provides an overview of qualitative baseline results collected from socially vulnerable patients and providers from three Canadian sites where organizational interventions have been implemented. This study provides insights on the needs of patients and providers to improve access to PHC care and to quality care in different contexts. It channels the input of providers and patients regarding main challenges to access for these patients and main barriers providers faced by providers when providing care.
Narrative-based Methodology for Qualitative Health Research: Ensuring Quality, Rigor, Consistency and Efficiency in a Mixed-Methods Health Research Evaluation Protocol
CAHSPR conference, Montreal
May 29, 2018
The aim of this presentation is to describe how narrative-based qualitative methods designed for a mixed-method evaluation protocol of interventions in Primary Health Care (PHC) can facilitate qualitative analysis in three different sites (Québec, Ontario and Alberta) to study interventions aimed to improve access to primary care for vulnerable populations.
Patient Navigation Integrated in Primary Care and Information Continuity
CAHSPR conference, Montreal
May 29, 2018
The objective of this poster is to describe an innovative patient navigation model integrated within primary care practices and how information continuity supports patients’ access to health enabling community resources (CR). We conducted a feasibility study to evaluate the potential for a navigation model (ARC) using non-clinical navigators to support patients with social challenges to overcome barriers to access CR. The ARC feasibility study suggests a model for integrating a navigator within primary care and the need to develop efficient communication strategies for patient access to CR.
Using an integrated knowledge translation (iKT) approach to develop a multi-site RCT protocol: The Access to Resources in the Community (ARC) study
CAHSPR conference, Montreal
May 29, 2018
This poster describes the integrated knowledge translation strategy used to inform the development of a complex intervention study aimed at assessing the impact of a non-clinical navigator integrated in primary care practices, on access to community resources for patients with social complexities. Grounded by the knowledge to action framework a comprehensive multi-site randomized control trial was developed using the engagement paradigm. Specifically, the study protocol was developed via formal consultations with patients, family members, providers (including multicultural health navigators) and with decision-makers. We also included feedback from a feasibility study conducted in four primary care practices in the Ottawa region.
Managing risk in navigation implementation research: an evidence-based project management approach
CAHSPR conference, Montreal
May 29, 2018
Using the ARC study, we demonstrate the value of conducting risk management prior to and throughout the conduct of implementation research projects to maximize the likelihood of delivery of the research as planned. ARC’s research aims to improve access to community resources in the Champlain LHIN region of Ontario. Steps included electronic anonymous individual consultations to identify, rate, and prioritize risks based on likelihood and impact, followed by consensual group discussions to design a risk management plan to optimize the conduct of the research.

Primary Health Care Needs Perception in Vulnerable Populations: A Qualitative Study in a Community Support Service
NAPCRG Conference, Montreal
November 20, 2017
IMPACT's south-east Melbourne intervention has sought to identify vulnerable clients of a Home and Community Care support program who lack access to enduring PC. A health broker is working with these clients to help gain access to an appropriate general practitioner. In contrast to what had been anticipated, the uptake of the program among the target group (those living with developmental disability, mental health conditions or epilepsy) has been low. The objective of this poster is to understand individual and contextual barriers to the recruitment of vulnerable clients to a health service broker intervention.

Evaluating a Pop-up Health and Community Event in Lethbridge, Alberta, Canada
NAPCRG Conference, Montreal
November 18, 2017
This poster presents one project within the IMPACT research program that focuses on implementing Pop-up health and community services events to support and improve access to primary healthcare (PHC) for vulnerable populations in Lethbridge, Alberta, Canada. The goal of the poster is to present the evaluation approach on outcomes for (1) patients; (2) service providers; and (3) the overall implementation of a reoccurring Pop-up intervention.

Knowing When, Where, Who and How to Engage in Participatory Action Research: Lessons From a Canadian-Australian Research Program That Aims to Improve the Access of Vulnerable People to Primary Healthcare Via Organizational Changes
NAPCRG Conference, Montreal
November 20, 2017
This poster reflects on the challenges, lessons learned, strategies, and structures developed to promote partner and patient engagement in long-term, complex primary health care interventions.

Community Based Health and Social Resources Recommended to Patients by Primary Care Providers
NAPCRG Conference, Montreal
November 18, 2017
In this poster, we present our study about a lay navigator that refers patients to community resources (CR). We undertook a primary care (PC) based study to improve patient access to CR. The goal is to promote integration of primary and community care to improve the utilization of CR.

Evaluating the Introduction of a Patient Navigator in Primary Care Practices: A Mixed Methods Approach
NAPCRG Conference, Montreal
November 18, 2017
This poster focuses on an intervention to facilitate appropriate referrals to community resources (CR) and provide access to a Patient Navigator that would 1. Improve provider awareness of and referrals to CR, 2. Improve patient access to CR, and 3. Enhance patient utilization of CR.

Multi-Stakeholder Partnerships to Promote Access to Primary Health Care for Vulnerable Populations: A Mixed Methods Study
NAPCRG Conference, Montreal
November 18, 2017
This poster shows preliminary results from the qualitative phase. It describes the intentional and emergent structures and processes used to develop and sustain multi-stakeholder partnerships within two local partnerships of an international research program entitled IMPACT;. It also analyzes how the structures and processes described above contribute to partnership effectiveness using the analytical lens of partnership synergy.

Cumulative Barriers to Access to Primary Care for People with Mental Health Conditions: Comparing Australia Internationally
PHCRIS Conference, Sydney
August 09, 2017
Variation in access to primary care has been demonstrated across countries, however there are gaps in assessing disparities for people with mental health conditions. Describing these is the aim of this presentation.
Barriers in access to PC were assessed in a secondary analysis of the 2016 Commonwealth Fund International Health Policy Survey. Within each of 11 countries, multiple logistic regression models were used to assess whether people with a mental health condition were more likely to experience multiple barriers in access to PC adjusting for age, sex, immigrant status, income, and other physical conditions.
Click Download Poster to learn more.

Health Service Brokers Facilitating Access to Primary Care: A Scoping Review
PHCRIS Conference, Sydney
August 09, 2017
This poster describes our scoping review process that aimed to assess (a) how brokers have been defined and described, (b) components of broker programs, and (c) to what extent patient-centredness, a dimension of high-quality primary care, has been incorporated into broker programs.
Twenty studies were included. None of these defined 'broker' or 'brokerage'. Studies provided a description of a broker-like person or, for three studies, a brokerage-like process. The components included activities to eliminate barriers to care and the broker as part of a coordinated system. Most studies had elements of patient-centred care: an informed and involved patient, receptive and responsive health professionals, and a coordinated, supportive environment.
Health services brokers may assist to connect people to appropriate primary care in a patient-centred way. Brokers require further study to determine their impact and cost-effectiveness, and patients' experiences of the brokerage process.

The Mental Health Care Gap: Comparing Access to Primary Care for People with and without a Mental Health Condition Across Developed Nations
PHCRIS conference, Sydney
August 08, 2017
This poster describes the contextual and organisational factors that may explain national differences in access for people with and without a mental health condition.
This mixed methods study presented data from the Commonwealth Fund 2013 International Health Policy Survey to international experts in primary care (policy makers, clinicians, researchers and community representatives). The interviews sought explanations for the quantitative findings were used to develop hypotheses about the potential explanations for variations in access to primary care in six western developed nations.
Our cross case analysis of the Commonwealth Fund data highlighted the importance of context (including geographic, demographic, health policy and organisation, funding, professional roles and workforce supply) in the provision of equitable services for this vulnerable population.

Multi-stakeholder Partnerships to Promote Access to Primary Health Care for Vulnerable Populations: A Mixed Methods Study
NAPCRG Conference, Colorado Springs
November 14, 2016
This poster examines the processes whereby diverse stakeholders work together in two PHC partnerships, in Quebec and Ontario; describes the work of these two partnerships with the analytical lens of partnership synergy; and quantitatively assesses the success of intentional and emergent processes and approaches to enhancing partnership synergy within these two partnerships.

Building backbone organizations to achieve collective impact: creating the foundation for achieving sustained change for primary healthcare transformation
NAPCRG Conference, Colorado Springs
November 15, 2016
This poster examines the collective Impact results when different stakeholders commit to a common agenda to solve a complex social issue. It describes the development of backbone organizations across the IMPACT program; to highlight similarities and differences in collaborative infrastructure; and, to discuss the influence of backbone organizations on implementation of community-based interventions.

Applying the Findings of a Rapid Realist Review to Inform the Planning for an Intervention to Increase Referrals from Primary Care to Community Resources
NAPCRG Conference, Colorado Springs
November 15, 2016
Under the IMPACT research program (Canadian-Australian collaboration to improve access to primary health care for vulnerable populations) the Ontario region prioritized improving access to primary health care resources, such as mental health and self-management programs to community members. Qualitative data indicated that primary care providers value these resources, but miss opportunities to refer because of poor awareness of programs, challenging referral processes, and a lack of integration of these sectors. The Ontario region commissioned a realist review to inform the development of an intervention to increase equitable access to community resources through primary care referral. This poster reports on that initiative.

Local Innovations From the IMPACT Program of Research: ARC Patient Navigation to support Equitable Access to Resources in the Community
NAPCRG Conference, Colorado Springs
November 15, 2016
Many community primary health care resources, such as self-management, smoking cessation and falls prevention programs, are severely undersubscribed. The constantly changing landscape of these resources, poor integration with primary care (PC) and their sheer number are such that most providers and patients are unaware of them. Electronic navigation tools exist to identify resources, but require high literacy and are largely unknown to providers and patients. Individuals with social barriers are especially vulnerable to poor access, and Francophones living in minority situations may face additional barriers. This poster examines the ARC Patient Navigation, a tool designed to support Equitable Access to Resources in the Community.

When science isn’t enough: The need to adapt to political and organizational evidence when designing an innovation to improve access to primary healthcare for vulnerable populations
NAPCRG Conference, Colorado Springs
November 15, 2016
IMPACT is a participatory action research program that aims to design, implement and evaluate local interventions to improve access to primary healthcare (PHC) for vulnerable populations in Canada and Australia. In Quebec, Canada, the intervention was designed by a partnership of researchers and PHC stakeholders over a two-year period during which many political and organizational changes took place. This poster presents how political, organization and scientific evidence informed the design of an intervention to improve access to primary healthcare for vulnerable populations.

Using Brokers to Link Vulnerable Individuals with Primary Care: A Scoping Review
NAPCRG Conference, Colorado Springs
November 15, 2016
Innovative Models Promoting Access-to-Care Transformation’ (IMPACT) is a collaborative research program that brings together clinicians, academics, community services and community members in six regions of Australia and Canada. IMPACT’s aim is to develop interventions to improve access to primary care for vulnerable people. One partnership, in Victoria, Australia, will use health brokers to link individuals to primary care services. This poster investigates how brokers have been defined, characterised and used to link individuals to primary care, and explores the extent to which recognised dimensions of patient-centred care are incorporated into broker interventions.

Engaging Patients for Primary Healthcare Intervention Research
NAPCRG Conference, Colorado Springs
November 15, 2016
This poster examines how patient engagement can help primary healthcare (PHC) researchers develop interventions that are relevant and acceptable to their target population. Many engagement strategies exist, but little is known about their effectiveness and appropriateness to engage vulnerable patients.

Utilising the RE-AIM framework in a realist review of health service brokerage
PHC Research Conference, Canberra
June 07, 2016
This poster is focused on a systematic review of health service brokerage. It forms part of the IMPACT (Innovative Models Promoting Access-to-Care Transformation) program with the aim of synthesizing evidence relating to access to e/m/telehealth interventions among vulnerable populations attending primary care.

Challenges in addressing and measuring access to care for vulnerable groups from a realist review of eHealth, mobile & telehealth interventions
PHC Research Conference, Canberra
June 07, 2016
This study was conducted in South Western Sydney, one of six research areas across Australia and Canada.
Within a rapid realist review we applied a conceptual framework to understand the impact of eHealth, mobile and telehealth interventions on access to primary healthcare for these population groups.
This review provides insight into the experience of vulnerable participants across the domains of access. The research found that e/m/telehealth interventions do have the capacity to ultimately improve access to primary healthcare for vulnerable populations.
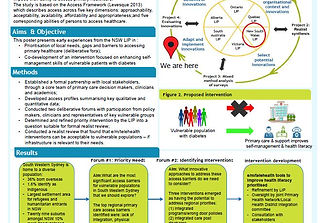
Co-creation of an Intervention to Improve Access for Vulnerable Populations
PHC Research Conference, Canberra
June 07, 2016
This poster presents early experiences from the New South Wales LIP in :
•Prioritisation of local needs, gaps and barriers to accessing primary healthcare (deliberative fora);
•Co-development of an intervention focused on enhancing self-management skills of vulnerable patients with diabetes

Health Service Brokers in Community-Based Primary Health Care: A Scoping Review
PHC Research Conference, Canberra
June 07, 2016
This poster presents the methodology for, and early findings from, a scoping review exploring how health brokers have been defined, characterised and used in primary health care. Additional analysis will explore the extent to which principles of patient-centred care have influenced these dimensions. The review question, ‘what is the extent and nature of the use of health service brokers’ has been answered, with a description of brokers, their components and patient-centredness.

Lessons Learned from Partnerships in the IMPACT Program
Health Services and Policy Research Conference, Melbourne
December 07, 2015
This poster focuses on lessons learned by the IMPACT team in setting up local partnerships to implement primary health care interventions that improve access for vulnerable communities. (Year 2 of 5)

Common Priorities and Common Innovations to Improve Access for Vulnerable Communities: Year 2 of the IMPACT Program
North American Primary Care Research Group conference, Cancun
October 25, 2015
This poster describes common primary health care access priorities and relevant intervention approaches in each region part of the IMPACT program.

Cross-Country Analysis to Identify Contextual Factors Associated with Inequalities in Access to Primary Care Among Vulnerable Populations
North American Primary Care Research Group conference, Cancun
October 26, 2015
This poster presents the mixed-methods approach the IMPACT team used to identify the organisational, system and contextual factors that influence access to primary health care for vulnerable populations.

Measuring Access to Primary Care Using International Surveys: A Mapping and Prioritising Process Based on the Commonwealth Fund International Health Policy Surveys
North American Primary Care Research Group conference, Cancun
October 27, 2015
This poster focuses on the IMPACT mixed methods research project with secondary analysis of 2013 and 2014 Commonwealth Fund International Health Policy Surveys. Using the data measuring access to care, we mapped questions to an established access framework and identified questions for quantitative analysis based on local priorities.

Promoting Access to Primary Health Care for Vulnerable Populations through Multi-stakeholder Partnerships
North American Primary Care Research Group conference, Cancun
October 25, 2015
This poster introduces the reader to Katya Loban's PhD project. The overall goal is to understand the effectiveness of multi-stakeholder partnerships in addressing complex issues in primary health care.

The Use of Social Media for Scoping Innovations in Primary Health Care: Lessons Learned from the IMPACT Study
North American Primary Care Research Group conference, Cancun
October 25, 2015
This poster describes how IMPACT developed a social media approach to identify innovative interventions aimed at improving access to primary health care for vulnerable populations.

IMPACTing on Access for the Vulnerable: An Evolving Community Partnership in South Eastern Melbourne
PHC Research Conference, Adelaide
July 29, 2015
This poster details Victoria's (Australia) partnership early experiences with two key components of the work: community engagement and priority setting. This presentation rests on early engagement and building collaborative relationships to foster ownership of a future intervention intimately aligned to regional need.

Measuring Access to Primary Care Using International Surveys
PHC Research Conference, Adelaide
July 29, 2015
This poster describes a method to identify contextual factors influencing equity in access to primary health care in 11 countries. The method is based on a deliberative approach involving community partners that enabled analysis of a reduced set of questions aligned with local priorities, from an initial list of over 50 questions mapped to five access domains.

An Ecological Model Promoting Access to Community-Based Primary Health Care for Vulnerable Populations
Primary Healthcare Partnership Forum, Newfoundland
June 29, 2015
This poster is based on the Alberta partnership experience. The goal of this presentation was to answer the question of whether a four-part ecological model promoting community development and capacity building can be used to promote access to Community Based Primary Health Care for vulnerable populations.

Creating Partnerships for Change: A Proposal to Study Multi-stakeholder Collaboration Towards Organizational Innovations to Promote Access to Primary Health Care for Vulnerable Populations
Canadian Association for Health Services and Policy Research Conference, Montréal
May 26, 2015
Using a scoping review, Katya Loban wishes, through her PhD project, to gain a deeper understanding of the effectiveness of multi-stakeholder partnerships in addressing complex issues in primary health care.

Transforming Primary Health Care Using Participatory Deliberative Processes for Collaborative Community Decision-Making
North American Primary Care Research Group Conference, New York
November 24, 2014
This poster explores how well the systematic use of a variety of deliberative processes across cases functions as a mechanism for meaningful engagement, knowledge exchange and collaboration. We report on the first phase of implementation of deliberative decision-making processes within the IMPACT partnerships.

Organizational Interventions Improving Access to Community-based Primary Health Care for Vulnerable Populations: a Scoping Review
North American Primary Care Research Group Conference, New York
November 22, 2014
This poster focuses on the scoping review method that was used to identify organizational innovations improving access to primary care services for vulnerable populations in the literature.

Innovations to Improve Access to Primary Health Care for Vulnerable Populations: Results from an Environmental Scan Using a Social Media Approach
North American Primary Care Research Group Conference, New York
November 24, 2014
In this poster, we report on findings from an innovative approach to capture emerging innovations designed to improve access to primary health care for vulnerable groups. The objective of the study was to identify and describe examples of innovative programs, services, approaches or models of care that have achieved better access to primary health care for vulnerable populations.

A Partnership Between Primary Care Researchers, Decision-makers and Community Members to Improve Access to Primary Health Care for Vulnerable Populations – The Ottawa (Ontario) Experience
North American Primary Care Research Group Conference, New York
November 24, 2014
This poster presents year 1 of the progress made in the Ontario partnership. They 1) established the partnership and identified the access information needs for their planning; 2) analyzed forty + relevant performance indicators across LHIN sub-regions and population strata; 3) disseminated findings to establish local access priorities.

Forum en médecine familiale, Québec
November 12, 2014
This poster describes IMPACT with the establishment of partnerships and the relationship between them and the research projects.